Glaucoma Treatment
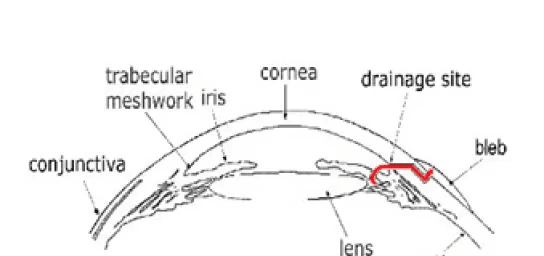
When glaucoma is refractory to medical therapy, laser therapy and surgical treatment are the options to consider. Dr. Seah is a Singapore Eye Specialist who has performed numerous glaucoma procedures including the complicated glaucoma drainage implant surgeries. With rich clinical experience in the treatment of glaucoma, he will be able to determine the best suited treatment for your condition.